Innovative Biosimilar Therapies for Multiple Myeloma
Explore the latest developments in biosimilar therapies for multiple myeloma, highlighting cost savings, regulatory advancements, and potential impact on treatment options. Discover how biosimilars may transform cancer care by providing effective but more affordable alternatives to biologics, with ongoing efforts to improve trust, regulation, and access within the healthcare industry.

Emerging Biosimilar Options for Multiple Myeloma Treatment
Multiple myeloma involves the malignant proliferation of plasma cells within the bone marrow, leading to skeletal damage, immune suppression, and kidney issues. Treatment strategies vary based on disease stage and include chemotherapy, steroids, targeted therapies, radiation, and stem cell transplants.
Treatment Costs and Advances
Over the past decade and a half, significant progress has been made in diagnosing and managing multiple myeloma, resulting in improved survival rates. However, the financial burden remains substantial, often exceeding costs associated with other cancer therapies.
The high expenses stem from multi-drug regimens, ongoing maintenance therapies, and the extended duration of care, which can total over $150,000 annually for initial treatment and about $100,000 for follow-up care. Introducing biosimilar drugs—copies of biologics with patent expirations—can potentially cut costs significantly, projecting savings of up to $54 billion between 2017 and 2026.
Biologics vs. Biosimilars
Biologics are advanced, targeted therapies derived from living organisms, revolutionizing cancer treatment by offering efficacy with reduced toxicity. Their complex production processes make them costly, and biosimilars—similar but not identical copies—can offer more affordable alternatives. Since biologics are intricate molecules like monoclonal antibodies, developing biosimilars involves overcoming significant manufacturing challenges.
Use of Biosimilars in Multiple Myeloma
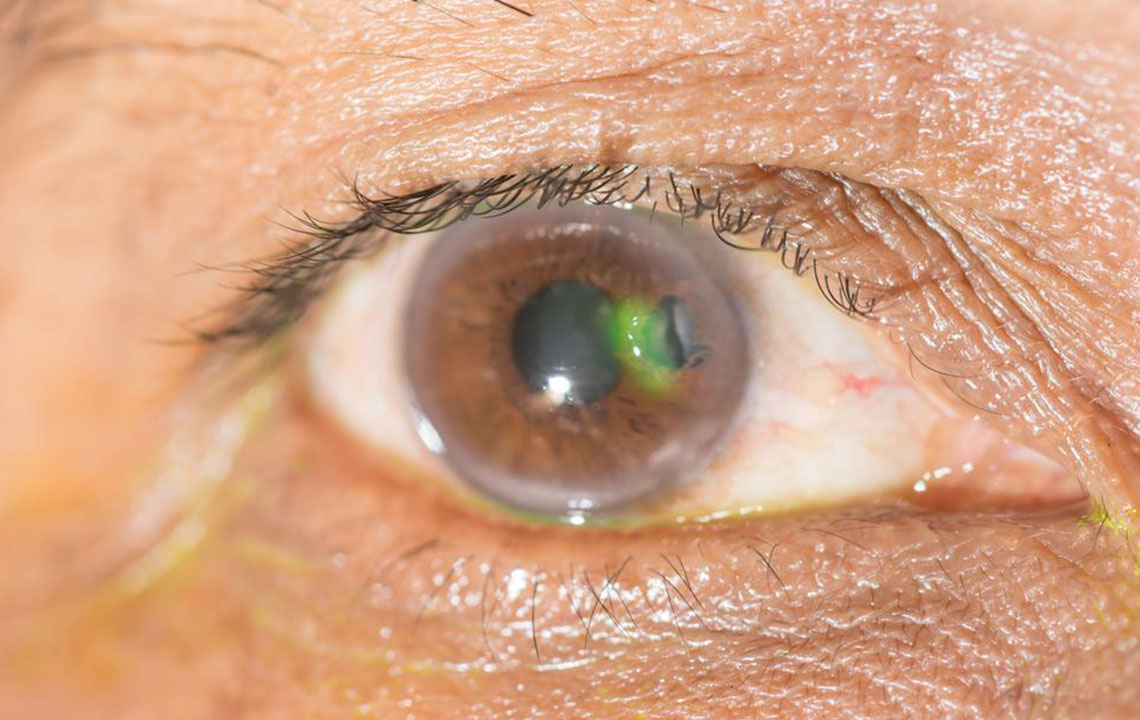
Despite promising potential, adoption of biosimilars for multiple myeloma faces hurdles. Medical professionals often hesitate due to limited clinical trial data, regulatory ambiguities, and concerns about immunogenicity. Clarification in approval processes, naming conventions, and insurance coverage is essential to boost confidence and adoption.
Efforts include education campaigns targeting healthcare providers and patients, emphasizing biosimilars' safety and efficacy. The American Society of Clinical Oncology has issued guidelines to advance understanding and integration of biosimilars into practice, ensuring safer and more cost-effective treatment options.
European countries have utilized biosimilars like Filgrastim and Epoetin since 2008, demonstrating improved patient access and treatment responses. In the U.S., the FDA plays a critical role by overseeing the evaluation and approval processes, ensuring biosimilars are safe, effective, and accessible.
FDA Regulatory Approach
The FDA's 351(k) pathway verifies biosimilar safety through rigorous testing. Recently, finalized guidance on interchangeable biosimilars allows substitution without prescriber intervention, further enhancing affordability and convenience.
Key biosimilars for multiple myeloma include Filgrastim, used to boost white blood cells prior to stem cell transplants, along with others like Thalomid, Revlimid, and Velcade.
Future of Biosimilars
The FDA's recent guidelines on interchangeability mark a milestone, potentially simplifying treatment by allowing pharmacists to automatically substitute biosimilars for originator biologics, pending prescriber approval. This development could revolutionize access and affordability in oncology care.