Understanding Meningitis Caused by Group B Streptococcus: Causes, Types, and Prevention Strategies
This article explores the causes, types, and prevention methods for meningitis caused by Group B Streptococcus. It highlights symptoms, risk factors, and essential preventive measures such as vaccination and hygiene practices. Early diagnosis and prompt treatment are emphasized to prevent severe complications like brain damage and death. The content offers a comprehensive overview suitable for individuals seeking to understand this serious infection and how to protect themselves or loved ones.

Understanding Meningitis Caused by Group B Streptococcus: Causes, Types, and Prevention Strategies
Meningitis involving Group B Streptococcus (GBS) refers to inflammation of the membranes surrounding the brain and spinal cord, known as meninges. This swelling often results in severe headaches, neck stiffness, and high fever. GBS-related meningitis can manifest in three forms: bacterial, viral, and fungal. The bacterial type is the most dangerous, potentially leading to paralysis, sepsis, strokes, or death if untreated. Recognizing the causes and symptoms is vital for early intervention.
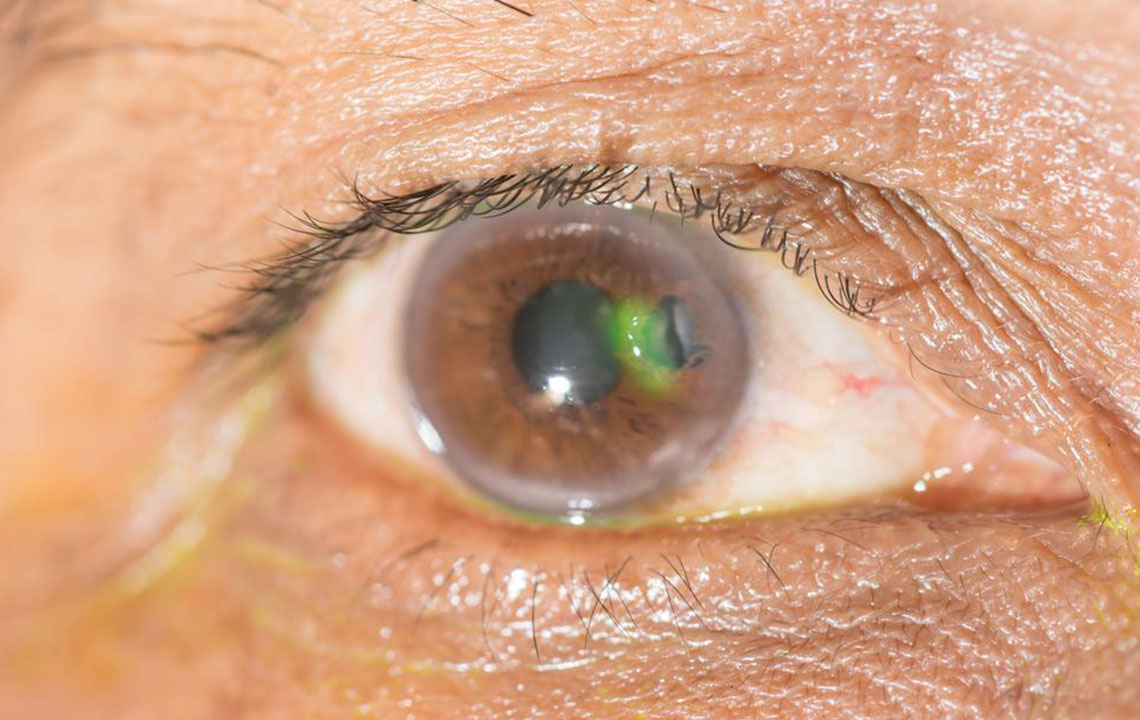
Transmission usually occurs through contact with bodily fluids like saliva or mucus, especially via coughing, sneezing, or sharing personal items. The bacteria travel through the bloodstream to infect the meninges, with initial symptoms resembling flu, such as neck stiffness, fever, nausea, confusion, seizures, or skin rash in severe cases. Prompt diagnosis and treatment are essential to prevent serious complications.
Types of Meningitis caused by GBS
Bacterial meningitis caused by GBS can progress rapidly, leading to permanent brain injury or death without timely treatment. It often follows sinus infections or head injuries, with strains like Streptococcus agalactiae being common culprits. It frequently affects newborns and immunocompromised individuals.
Viral meningitis results from infections such as HIV or mumps. Usually less severe, it often resolves on its own but requires caution to prevent chronic issues.
Fungal meningitis mimics bacterial forms but isn't contagious; it is life-threatening if not treated with antifungal medications.
Risk factors include:
Weakened immune system due to diseases like AIDS or cancer
History of head injuries or previous meningitis episodes
Recurrent respiratory illnesses
Chronic illnesses like liver or heart disease
Skipping recommended vaccinations
Prevention tips
Stay updated with vaccinations such as the Hib vaccine, meningococcal conjugate vaccine, and pneumococcal vaccine.
Maintain good personal hygiene by washing hands regularly and avoiding sharing personal items like utensils and toothbrushes.
Cover your mouth and nose when sneezing or coughing to prevent spreading germs.
Eat a healthy diet rich in vegetables and exercise regularly to boost your immune system.
Effective treatment depends on identifying the infection's cause and severity. Bacterial infections require immediate hospital admission and intravenous antibiotics to prevent serious neurological damage. Fungal infections are treated with antifungal drugs, while viral cases often resolve naturally or need supportive care. Early diagnosis and follow-up care are vital to avoid long-term complications such as memory loss, sensory deficits, or neurological issues.