Understanding Vaginal Dryness During Menopause: Causes, Symptoms, and Solutions
Menopause-associated vaginal dryness is common but often overlooked. This article covers its causes, symptoms, diagnosis procedures, and effective treatments such as topical estrogen, lubricants, and lifestyle changes. Consulting a healthcare professional is essential for personalized management. Understanding and treating menopause-related dryness can greatly improve comfort and wellbeing during this phase of life.

Understanding Vaginal Dryness During Menopause: Causes, Symptoms, and Solutions
Vaginal dryness is a widespread concern among women experiencing menopause. Unfortunately, many are unaware that effective treatments exist, leading them to avoid seeking medical advice. This condition can cause discomfort during intimacy, reduce sexual desire, and make physical activities uncomfortable, increasing infection risks. This article explores the causes, symptoms, diagnosis methods, and available remedies for menopause-related vaginal dryness.
What leads to dryness during menopause?
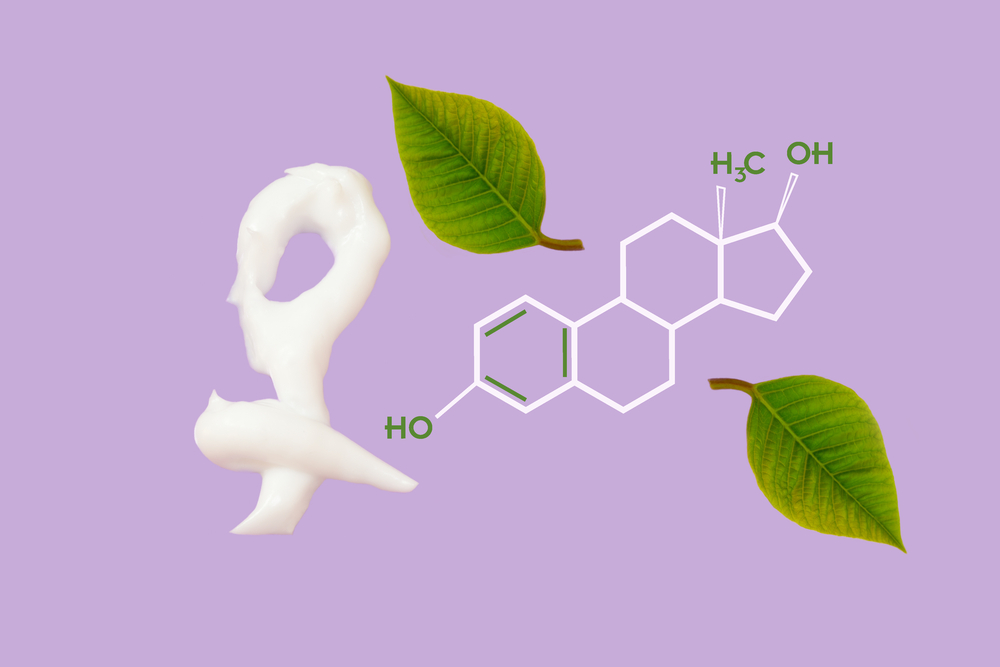
The vaginal walls are lubricated by a clear fluid maintained by estrogen. This hormone ensures the tissues stay thick, elastic, and healthy.
This hormone, produced by the ovaries, influences many bodily functions, including breast development, body shape, pregnancy, and menstrual regulation. As women approach menopause, estrogen levels decline, decreasing vaginal moisture and resulting in dryness. While hormonal fluctuations can cause this at any age, it's more common in older women. Symptoms range from mild irritation to severe discomfort, impacting daily life.
How can you tell if menopause is approaching?
During transition phases, women may notice irregular periods, hot flashes, sleep issues, mood swings, declining fertility, and urinary problems. The peri-menopausal period usually begins between ages 45 and 55 and lasts up to 14 years. Post-menopause, symptoms like vaginal dryness, itching, recurrent infections, painful intercourse, and urinary issues such as burning and incontinence are common. The vaginal canal may also shrink and tighten, causing soreness and discomfort.
Other causes of vaginal dryness besides menopause
Beyond menopause, factors like childbirth, breastfeeding, chemotherapy, radiotherapy, anti-estrogen medications, and surgical removal of ovaries can reduce estrogen and cause dryness. Autoimmune conditions like Sjogren syndrome affecting tear and saliva glands can also play a role. Medications such as antihistamines, which dry secretions, can lead to vaginal dryness and urinary issues. Stress and certain treatments might likewise lower estrogen, leading to similar problems. Regardless of cause, menopause-related dryness can cause burning, itching, and painful intimacy. Lifestyle choices speeding up menopause may exacerbate dryness, but treatments are available. Consulting a doctor is recommended for diagnosis and personalized solutions.
How is menopause-related dryness diagnosed?
If experiencing discomfort, burning, or itching, scheduling an appointment with a gynecologist is essential. The doctor will review health history, symptoms' duration, and triggers. A pelvic exam may be performed to assess tissue thinning or redness, helping rule out infections. A Pap smear might be performed to examine cells from the cervix or vaginal wall for further insights.
Remedies for menopause-related dryness
Addressing dryness is crucial for improving quality of life. Following professional guidance, women can consider these remedies:
Estrogen creams or gels: Topical estrogen formulations can effectively soothe dryness and irritation when applied directly to the vaginal area.
Oral estrogen therapy: While less targeted, oral options can supplement estrogen levels but should only be used under medical supervision due to possible side effects.
Moisturizers and lubricants: Water-based lubricants during intercourse can reduce discomfort. Regular vaginal moisturizers help maintain natural moisture if used consistently.
Engaging in regular intimacy: Sexual activity increases blood flow, supporting natural lubrication and tissue health.
Vaginal dryness may begin early in menopause and, if untreated, impact daily comfort but typically does not threaten health. Professional consultation and appropriate remedies can offer significant relief.
Note:
This site offers information across various health topics. While well-researched, readers should consult healthcare professionals for personalized advice. We do not guarantee accuracy or completeness and remind users that different platforms may present varied data or offers.