Essential Guidelines for Managing Seizures Effectively
This article provides comprehensive guidelines on managing seizures, including causes, risk of recurrence, treatment options, and emergency protocols. It emphasizes timely medical intervention, medication strategies, and the importance of regular follow-up. Whether dealing with initial seizures or recurrent episodes, understanding these management practices is vital for patient safety and prevention of long-term neurological complications.

Essential Guidelines for Managing Seizures Effectively
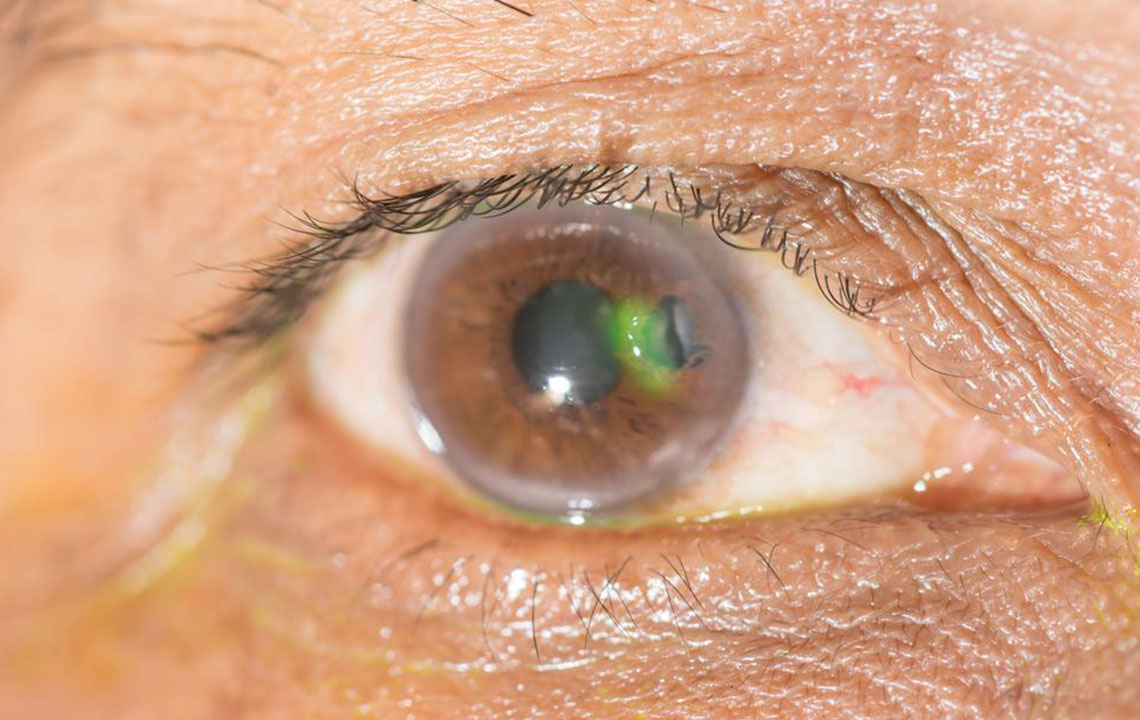
A seizure results from an imbalance between brain cells that excite and those that inhibit activity. Normally, the brain maintains a balance between these cells communicating and sending signals. Seizures are temporary, lasting minutes, but can sometimes trigger a surge of electrical activity that affects brain function, potentially causing paralysis or other neurological issues. Some seizures are subtle and easily overlooked, while others can lead to significant neurological impairments.
When is a seizure likely to recur?
Individuals who have experienced a seizure are at high risk of having another within six months.
If the cause of the initial seizure is identified accurately, recurrence is very probable.
Patients with multiple seizures are likely to have future episodes.
Seizures resulting from brain injury or infection can progress into epilepsy.
Seizure management protocols
While seizures can sometimes lead to paralysis, they can also pose life-threatening risks if prolonged beyond 30 minutes. Prompt and appropriate medical intervention can be life-saving. The American Epilepsy Society has established treatment protocols aimed at preventing future seizures and safeguarding patient health. Some patients may not respond fully to treatments or experience side effects. The primary approaches are monotherapy, which involves a single medication and is preferred, and polytherapy, which combines multiple drugs but can be costlier and have more side effects. Psychosocial support is also crucial for recovery.
Even with therapies, lifelong fear of recurrence persists. Patients should consult neurologists or epileptologists regularly and consider EEG monitoring. Consulting neurosurgeons is also recommended for comprehensive care.
Likelihood of seizure recurrence
Patients with a single seizure may avoid anticonvulsants and focus on lifestyle changes like avoiding alcohol and ensuring sufficient sleep.
Multiple seizures usually necessitate ongoing medication to prevent recurrence.
The American Epilepsy Society recommends a four-stage process for seizure treatment:
0–5 minutes: Stabilization and initial assessment.
5–20 minutes: Initiate treatment with benzodiazepines.
20–40 minutes: Administer medications like fosphenytoin, valproic acid, or levetiracetam if needed.
Beyond 40 minutes: Use anesthetic medications such as thiopental or propofol if seizures persist.
In critical cases, intensive care and rapid intervention are essential to prevent neurological damage. Prolonged seizures pose significant risks, emphasizing the importance of early treatment.
Seizures occur due to abnormal electrical activity in the brain, leading to symptoms like body shaking or unconsciousness. Immediate medical intervention is vital. Treatments include medication and sometimes surgery, but success varies. Underlying causes can be genetic or related to metabolic imbalances, while triggers may include brain injury or stroke. Regular medical follow-up and monitoring are crucial for managing this condition effectively.