Comprehensive Guide to Managing Chronic Bronchitis
Chronic bronchitis is a long-term lung condition characterized by persistent cough and mucus production. This guide explains its causes, risk factors, symptoms, diagnosis, and treatment options, emphasizing the importance of quitting smoking and seeking specialized care to manage the disease effectively.

Understanding Chronic Bronchitis: Causes, Symptoms, and Treatment
While typical colds or flu resolve within weeks, some individuals develop persistent lung issues like bronchitis. This condition involves inflammation and swelling of the bronchial tubes, the passages that channel air into the lungs, leading to chronic cough and excess mucus. Bronchitis can manifest as either acute or chronic.
Acute bronchitis is common and typically lasts a few weeks, with minimal long-term effects. In contrast, chronic bronchitis is a severe, recurring condition that persists or worsens over time.
Chronic bronchitis is part of the broader chronic obstructive pulmonary disease (COPD) spectrum. It involves ongoing inflammation of the larger airways, producing excess mucus that hampers breathing and triggers coughing.
Defined by daily mucus production and a cough lasting at least three months over two consecutive years, chronic bronchitis is often triggered by cigarette smoking, long-term exposure to fumes, air pollution, or dust. It's a persistent condition that may relaps or never fully resolve.
Risk Factors for Chronic Bronchitis
Smoking: The primary cause of chronic bronchitis.
Environmental Pollution: Long-term exposure to fumes, dust, or air pollution can contribute.
Genetics: Family history may increase susceptibility.
Repeated Respiratory Infections: While not a cause, infections can worsen symptoms and prolong the disease.
Signs and Symptoms
Persistent cough with mucus
Chest discomfort or tightness
Colored sputum (green, white, or yellowish-gray)
Occasional fever and chills
Fatigue and weakness
Shortness of breath
Chronic bronchitis involves mucus-producing coughs for at least three months annually over two years. Flare-ups may occur, indicating an acute infection overlaying the chronic condition.
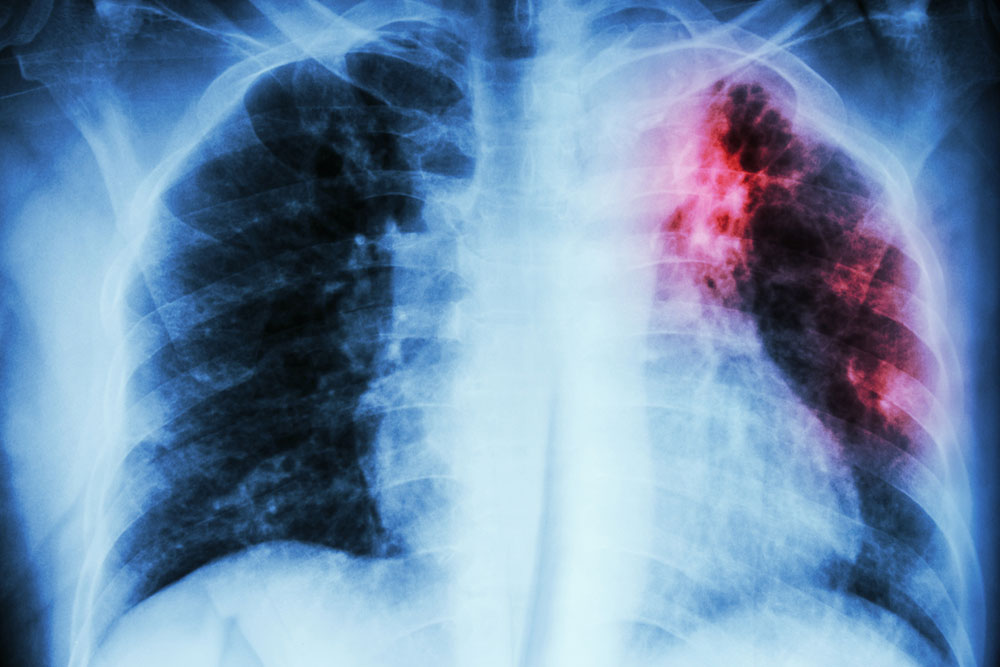
Diagnosis Methods
Blood analysis
Chest radiographs
ECG tests
Pulmonary function tests
Blood oxygen levels
High-resolution CT scans
Treatment Approaches
Effective management centers on reducing airway obstruction. Smoking cessation is crucial; it slows disease progression and extends lifespan. Oxygen therapy may be needed in advanced cases. Typical treatments include:
Medications: Bronchodilators, corticosteroids, and antibiotics to control symptoms and prevent exacerbations.
Rehabilitation: Chest physiotherapy improves mucus clearance and overall quality of life.
Oxygen Therapy: Used for severe airflow limitation, delivered via masks or nasal prongs.
Additional Measures: Annual flu and pneumococcal vaccines help reduce infection risks. For right heart failure complications, diuretics might be prescribed.