Comprehensive Guide to Managing Diarrhea Predominant IBS (IBS-D)
This guide offers an in-depth look into IBS-D, exploring its causes, symptoms, and management strategies. Learn how lifestyle changes, diet adjustments, and stress management can alleviate symptoms. Discover effective ways to improve digestive health and quality of life. Perfect for those seeking comprehensive information on IBS-D to make informed health decisions.

Understanding and Managing IBS-D
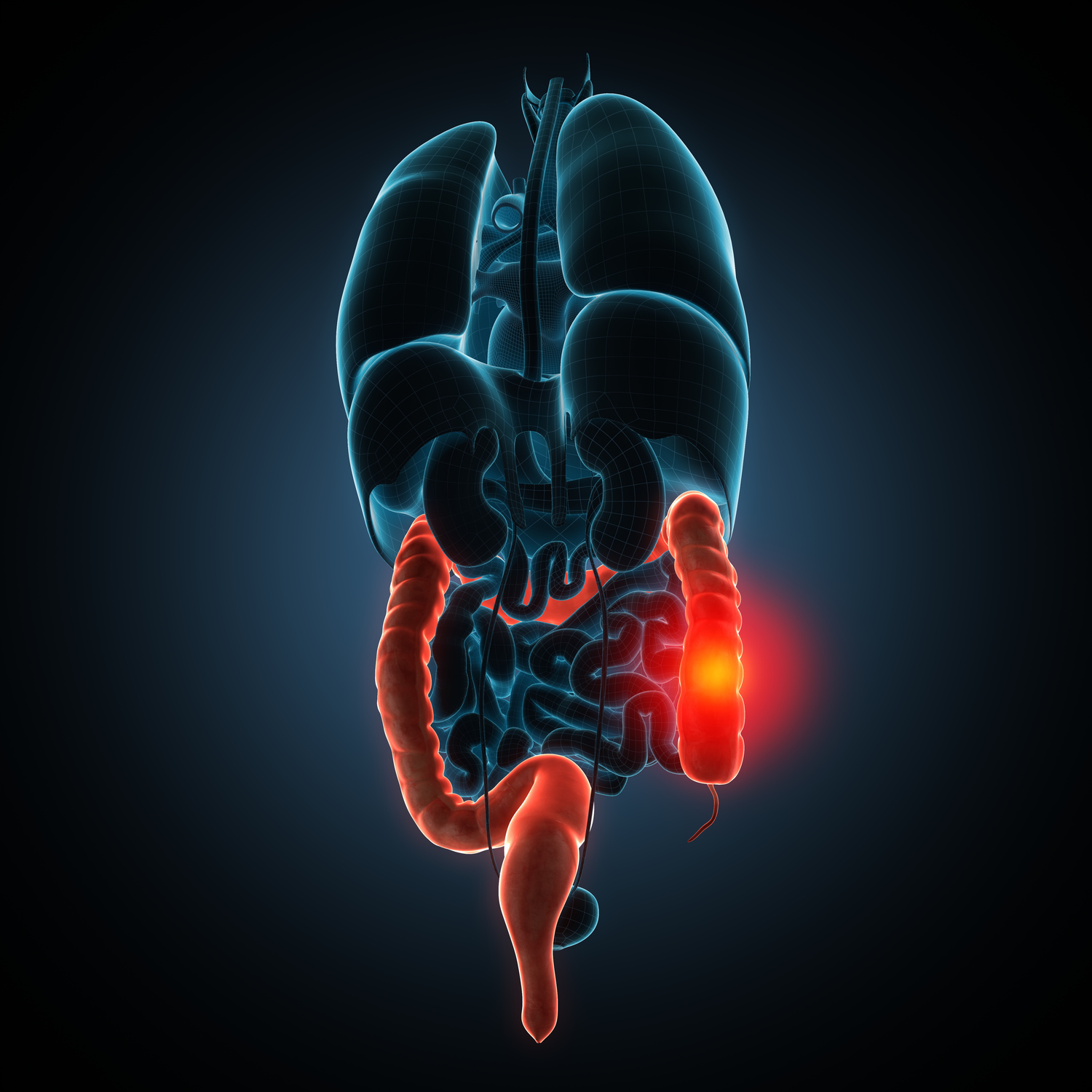
IBS, or Irritable Bowel Syndrome, primarily affects the large intestine and impacts millions globally, including around 25-45 million Americans. Typically, those in their late teens to early 40s are most at risk. Symptoms often include abdominal pain, discomfort, irregular bowel movements, bloating, mucus in stools, and excessive gas. Though not life-threatening, IBS-D requires consistent management, healthy lifestyle choices, and therapeutic intervention to control symptoms effectively.
Healthcare providers categorize IBS into three types: IBS-D with diarrhea, IBS-C with constipation, and IBS-M with mixed symptoms.
IBS-D – diarrhea as the main issue
IBS-C – primarily constipation
IBS-M – alternating symptoms of diarrhea and constipation
Causes of IBS-D
While the exact origins of IBS-D remain unclear, several factors influence its development:
Intestinal muscle activity
The digestive tract relies on muscle contractions to move food forward. Excessively strong contractions can cause bloating, gas, and diarrhea, whereas weaker movements lead to slow transit and hard stools.
Nervous system irregularities
Abnormal nerve responses in the gut can cause hypersensitivity, resulting in discomfort, pain, or irregular bowel habits.
Inflammation in the gut
Increased immune cell presence in intestinal walls can cause inflammation, contributing to symptoms like diarrhea and constipation.
Infections
Severe bacterial infections or bacterial overgrowth can predispose individuals to IBS-D.
Triggers for IBS-D
Certain factors can exacerbate symptoms, including:
Foods such as refined grains, processed items, dairy, and certain vegetables
Stresses from daily life or psychological distress
Hormonal fluctuations, especially in women during menstruation
Poor lifestyle habits like irregular sleep, unhealthy diets, and erratic routines.
Stress notably worsens IBS-D symptoms by affecting gut motility and sensitivity. Hormonal changes can also trigger or intensify episodes, especially in women. Moreover, a sedentary or unhealthy lifestyle can influence symptom severity.
Managing and Treating IBS-D
Diagnosis is primarily based on symptom assessment and medical history; there is no definitive test for IBS-D. Treatment focuses on relieving symptoms through lifestyle and diet adjustments, stress management, and sometimes medication.
Dietary modifications include avoiding gas-producing foods like carbonated drinks, caffeine, and certain fruits and vegetables. Some individuals see improvement after eliminating gluten from their diet.
Adopting simple lifestyle changes can be effective. These include consuming fiber-rich foods, maintaining consistent meal times, and engaging in regular exercise.
Understanding triggers and making these changes can significantly improve quality of life. Although medications exist, a combination of healthy eating, physical activity, and stress control often helps manage symptoms effectively, promoting overall well-being.