Understanding the Variations and Types of Amyloidosis
Amyloidosis is a rare but serious condition involving abnormal protein deposits affecting multiple organs. This article explores its main types, symptoms, and importance of early diagnosis. Recognizing the specific form can significantly influence treatment decisions and prognosis, helping patients manage this potentially life-threatening disease more effectively. Advances in research continue to improve understanding and treatment options for amyloidosis, making awareness crucial for at-risk individuals.
Understanding the Variations and Types of Amyloidosis
Amyloidosis is a rare and complex disease characterized by abnormal protein deposits called amyloid accumulating in various organs. Though medical advancements have been made, there is no universal cure, making early detection and management crucial. This condition can impact vital organs including the heart, kidneys, liver, and nervous system, potentially leading to organ failure. Recent scientific studies have improved our understanding of its subtypes, aiding in tailored treatment approaches. Recognizing the specific type of amyloidosis is essential for effective management and prognosis.
Amyloidosis occurs when amyloid proteins deposit in tissues and organs, disrupting normal function. These abnormal proteins originate from the bone marrow and can target various body parts. Due to its potential severity, correct identification of the disease type is vital, guiding treatment options and improving outcomes.
Major Types of Amyloidosis
AL (Primary) Amyloidosis AL amyloidosis, the most prevalent form, results from abnormal plasma cells producing misfolded light-chain antibodies. These proteins circulate in the bloodstream and deposit in organs like the heart, kidneys, and nervous system, often associated with multiple myeloma. Damage to these organs can be severe if untreated.
AA (Secondary) Amyloidosis This type arises due to prolonged inflammation or infection, triggering the production of serum amyloid A protein. Conditions such as rheumatoid arthritis or persistent infections like tuberculosis can lead to amyloid buildup, primarily affecting kidneys, liver, and spleen.
Familial and ATTR Amyloidosis Inherited mutations cause this form, particularly affecting transthyretin (TTR). The mutant protein forms amyloid fibrils that typically target the heart and nervous system. Although serious, genetic screening can identify at-risk family members, helping in early diagnosis and management.
Senile Systemic Amyloidosis Like familial types, this involves normal transthyretin but deposits develop gradually with age, mainly affecting individuals over 65. Because deposits accumulate slowly, the prognosis tends to be better than other types.
Dialysis-Related Amyloidosis Common among long-term dialysis patients, this form stems from beta-2 microglobulin deposits, often affecting bones, joints, and tendons.
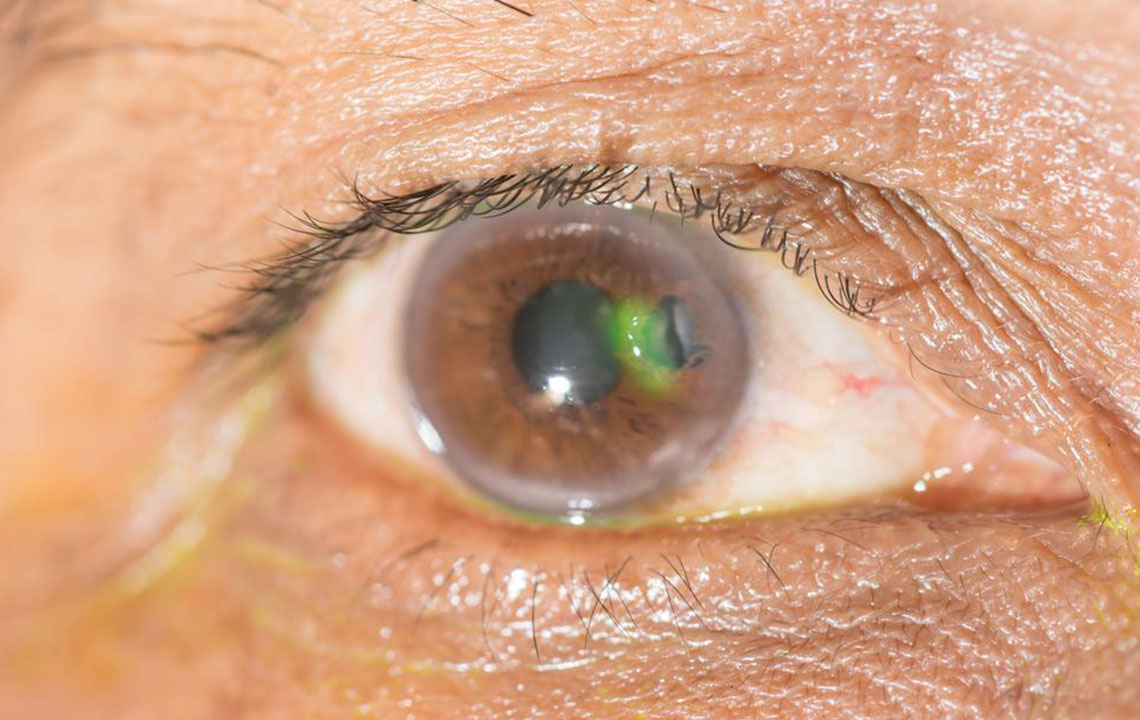
Organ-Specific Amyloidosis Deposits confined to a single organ, such as the skin, characterize this form. While some amyloid types are linked to diseases like Alzheimer’s, the brain is rarely involved.
Early identification of the amyloidosis type is vital to managing this life-threatening condition effectively and improving patient outcomes.