Understanding Clotting Disorders: Symptoms, Causes, and Management
Discover comprehensive insights into blood clotting disorders, including symptoms, causes, diagnosis, and natural management options. Learn how genetic and acquired factors contribute to abnormal clot formation, and explore lifestyle tips to support blood health. Early detection and medical consultation are crucial for effective management of these potentially serious conditions.
Understanding Clotting Disorders: Symptoms, Causes, and Management
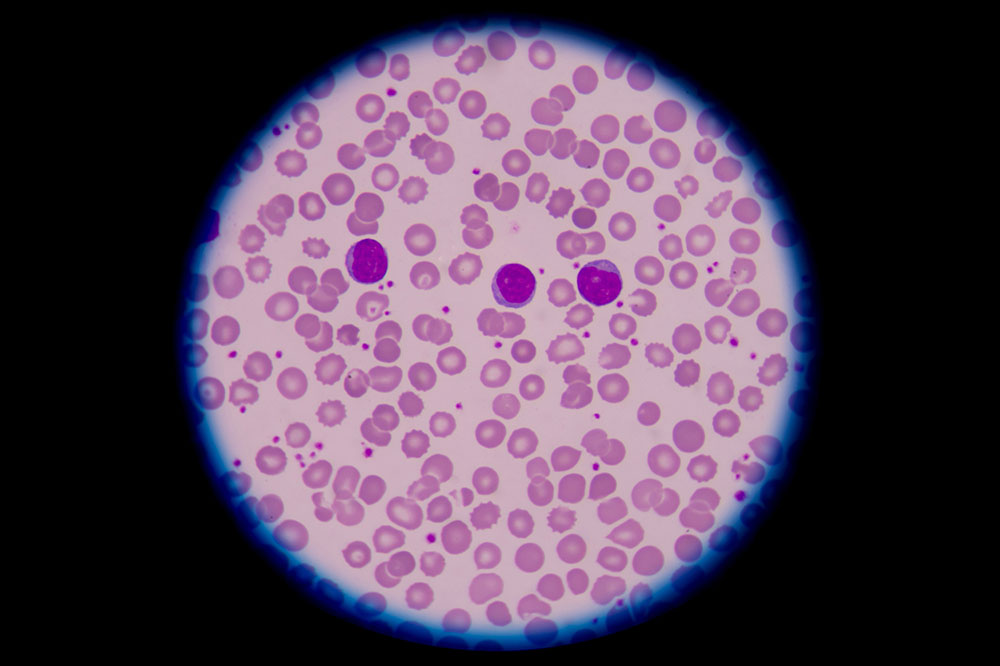
Blood clotting is essential to stop bleeding after an injury. Platelets and proteins in the blood work together to form a clot during coagulation, which typically dissolves naturally once healing occurs. However, some individuals have conditions that disrupt this process, leading to abnormal clot formation or delayed healing.
What are bleeding and clotting abnormalities?
These disorders involve either excessive clotting within blood vessels without injury or difficulty forming clots after injury, posing serious health risks.
The medical term for excessive clotting is hypercoagulability or thrombophilia, which can be life-threatening if not identified promptly.
Individuals with such conditions can develop clots in arteries and veins throughout the body. Clots near the heart increase risks of stroke and heart attacks. The location of clots determines their specific names; for example, deep vein thrombosis (DVT) describes clots in leg veins, often causing swelling and pain. Pulmonary embolism involves clot formation in the lungs, leading to severe complications.
Many with clotting issues show no symptoms, but signs such as chest pain, rapid breathing, shortness of breath, or fatigue may indicate a clot. Leg clots often cause calf swelling and tenderness. Anyone experiencing these symptoms should consult a healthcare professional for diagnosis.
Clotting disorders can be inherited or acquired. Genetic cases involve conditions like factor V Leiden mutation, abnormal fibrinolytic activity, or protein deficiencies that promote clot formation from birth. Acquired factors include surgeries, trauma, pregnancy, hormone therapy, prolonged bed rest, infections, or chronic illnesses like cancer and heart disease.
Diagnosis involves detailed medical history review and blood tests. Doctors assess for early-onset clotting, recurrent episodes, or family history. Laboratory tests such as PT (prothrombin time) and aPTT (activated partial thromboplastin time) measure blood clotting time. Specific genetic tests and antibody screenings determine inherited or acquired causes.
While medical treatment is essential, certain lifestyle and dietary changes may assist in managing clot risk. Incorporating turmeric, garlic, and cayenne peppers into meals can support blood health due to their natural properties. Turmeric contains curcumin, which helps prevent clots and reduce pain. Garlic's sulfur compounds aid in clot dissolution and lower blood pressure. Cayenne peppers have salicylates that naturally thin the blood, but should be used in moderation due to their spiciness.