Key Health Conditions Requiring Blood Donations
This article highlights common health conditions that require blood donations, including trauma, infections, and blood disorders like anemia, leukemia, and hemophilia. It emphasizes the importance of blood transfusions in managing severe injuries, chronic illnesses, and genetic disorders. Understanding these conditions underscores the vital role of blood donations in saving lives and supporting treatments worldwide.

Key Health Conditions Requiring Blood Donations
Reasons for Blood Transfusions
Every year, countless blood transfusions are performed for a variety of medical reasons. R
Major injuries and surgeries
Blood donations are vital after severe accidents like car crashes or natural disasters that lead to significant bleeding. A single car accident victim may require up to 100 pints (4.5 liters) of blood. Blood is also essential for war casualties and surgical procedures involving substantial blood loss.
Infections
Certain serious infections impair the body's ability to produce vital blood components.
Blood disorder conditions
Red Blood Cell Diseases
Anemia: This condition results from a shortage or abnormality of hemoglobin— the component carrying oxygen in red blood cells. Symptoms include fatigue and weakness. Severe anemia often necessitates blood transfusions to replenish healthy red blood cells.
Iron-deficiency anemia: In critical cases, transfusions provide immediate iron and red blood cells to improve symptoms temporarily, though further treatment is necessary for full recovery.
Aplastic anemia: Bone marrow failure causes a reduction in all blood cells. Blood transfusions help manage symptoms and prevent bleeding, but long-term treatment may involve immunosuppressive medication and iron removal therapies.
Chronic diseases causing anemia: Conditions like Crohn’s disease, lupus, and rheumatoid arthritis can lead to anemia. Transfusions alleviate severe symptoms in such cases.
Thalassemia: An inherited disorder common in Asian and African populations, necessitating regular blood transfusions to maintain healthy red blood cell levels. Iron chelation may also be needed to prevent iron overload.
Sickle cell disease: This inherited disorder causes misshapen hemoglobin, obstructing blood flow. Transfusions assist in managing complications like severe anemia but do not cure the disease.
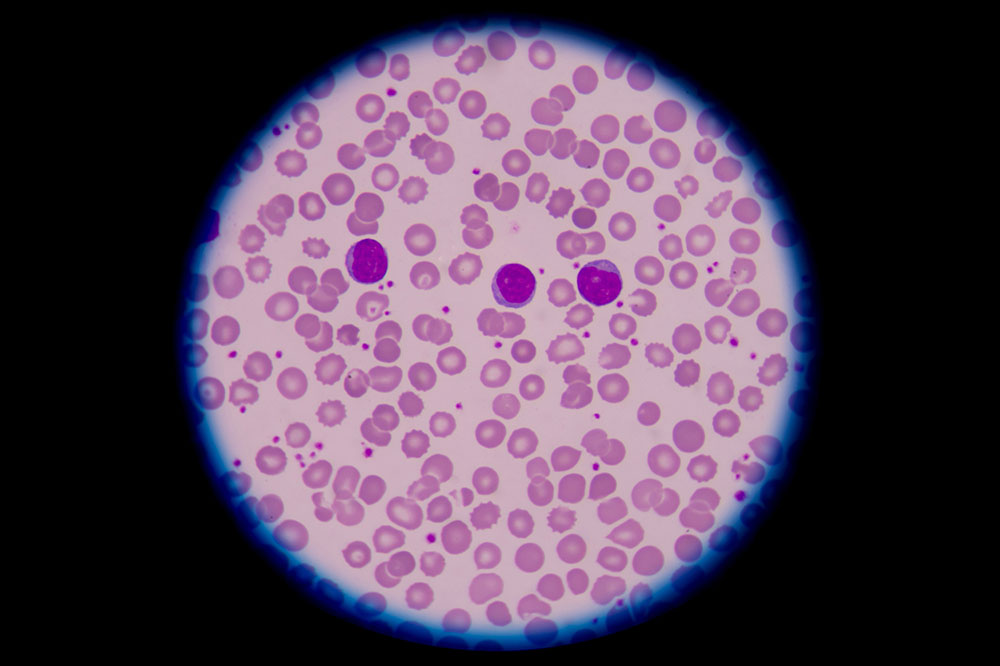
White Blood Cell Disorders
Lymphoma: Cancer of the lymphatic system, impacting immune response.
Leukemia: A blood cancer originating in bone marrow or lymph tissue, leading to abnormal white cell proliferation.
Multiple myeloma: Malignant plasma cells produce harmful proteins, often requiring transfusions to support blood cell levels during treatment.
Myelodysplastic syndromes: Bone marrow produces insufficient mature blood cells, often treated with red blood cell or platelet transfusions to control bleeding and anemia.
Platelet Deficiency Conditions
Thrombocytopenia: Conditions like heparin-induced thrombocytopenia cause a low platelet count, sometimes necessitating transfusions during bleeding episodes.
Plasma Disorders
Hemophilia: An inherited deficiency of clotting factors, leading to excessive bleeding that can be managed with plasma-derived clotting factor transfusions.
Von Willebrand disease: A protein deficiency impairing clot formation, treated with plasma products to control bleeding.
Major Blood Loss Situations
Significant blood loss occurs in various situations. Notably, postpartum hemorrhage is a major concern, with blood loss exceeding 500 mL after vaginal delivery and 1,000 mL after cesarean. While well-managed in developed regions, many areas still rely on blood transfusions to save lives.
Note: This blog offers diverse medical information based on research and data analysis. While informative, it should not replace professional medical advice. The site disclaims liability for data inconsistencies or additional offers beyond the presented content.